Suicide in Teenagers
Supporting suicidal teens requires flexible care, family involvement, and close attention to emotional progress.

Dr. Amir Elsamadisi
Psychiatrist & Researcher

Treating Suicidal Teens: Why the TASA Study Proves There’s No One-Size-Fits-All Solution
Description:
After a teen survives a suicide attempt, the next steps are critical — but also deeply complex. The TASA Study (Treatment of Adolescent Suicide Attempters), published in the Journal of the American Academy of Child & Adolescent Psychiatry, tracked teens after hospitalization for a suicide attempt. It asked tough questions: Who’s most at risk for another attempt? What kinds of treatment actually help? And how can we better support these teens as they heal? The answers weren’t always simple — but they were powerful.
The Takeaway
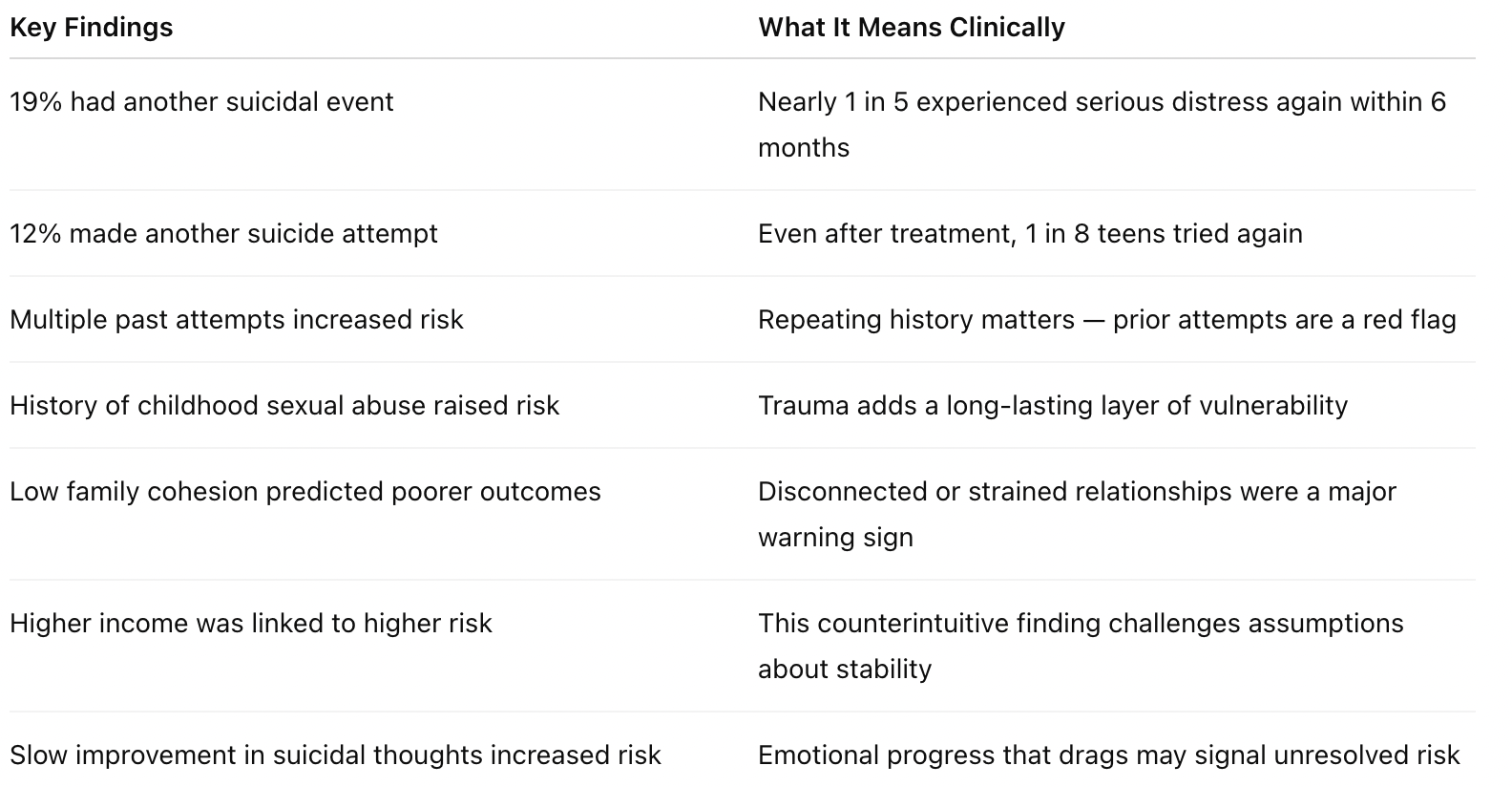
There’s no easy roadmap for helping suicidal teens — but there is hope. The TASA study followed 124 teens after a suicide attempt and found that:
- 19% had another suicidal event
- 12% made another suicide attempt
Several risk factors made future attempts more likely:
- A history of multiple prior attempts
- Childhood sexual abuse
- Low family cohesion (strained or distant family relationships)
- Higher household income, surprisingly, was also linked to increased risk
- And most striking: teens whose suicidal thoughts decreased slowly over time were more likely to try again — showing that stalled emotional progress can be a warning sign
In short: healing is possible, but it’s never linear. Progress takes time, and what works varies from person to person.
Why Should You Care
Teen suicidality is rising — and it often doesn’t look how we expect. This study found that 12% of teens attempted suicide again within 6 months, despite receiving treatment. That means checking in once isn’t enough. Healing takes ongoing, connected care that flexes with the teen’s needs.
The Article
The TASA study is a robust, multi-site, open-label observational trial published in JAACAP. It didn’t test one magic solution — instead, it reflected real-life treatment as it’s often practiced: some teens received Cognitive Behavioral Therapy (CBT), others were prescribed antidepressants (SSRIs), and many received both. The strength of this study lies in how closely it mirrors the complexity of real clinical practice. It gives us a realistic, unvarnished look at what recovery can actually look like.
The Clinical Data
Here’s what the study found among the 124 teens tracked after a suicide attempt:
Study Design: How They Figured This Out
- Study Name: TASA (Treatment of Adolescent Suicide Attempters)
- Type: Open-label, multi-site observational study
- Participants: 124 teens recently hospitalized after a suicide attempt
- Treatments Used: Cognitive Behavioral Therapy (CBT), SSRIs (antidepressants), or both
- Duration: 6-month follow-up period
- Published in: Journal of the American Academy of Child & Adolescent Psychiatry (JAACAP)
The researchers tracked suicidal events, therapy engagement, and emotional progress over time — capturing what worked and what didn’t in the real world.
Why This Study Changed My Practice
Before reading TASA, I wanted suicide risk to feel more clear-cut. I hoped certain symptoms would tell me exactly who needed more support. But this study taught me otherwise. Risk isn’t always obvious, and recovery doesn’t follow a straight line.
Now I tell families:
“Improvement that stalls is just as concerning as symptoms that worsen. We don’t just treat the crisis — we stay present during the quiet after.”
TASA reminded me to:
- Look for subtle signs, not just overt symptoms
- Engage families as active partners — not observers
- Avoid cookie-cutter treatment plans — flexibility matters
- Treat progress plateaus as potential warning signs
Supporting suicidal teens takes more than checklists. It takes trust, time, and personal connection.
What Parents Should Know
- Recovery takes time. Healing after a suicide attempt is rarely fast — but it’s possible.
- Combination treatment helps. Many teens do best with both medication and therapy.
- Don’t ignore slow progress. If suicidal thoughts linger or improvement stalls, speak up.
- Family support protects. Strong relationships and open communication can make a huge difference.
- Your role matters. Parents aren’t just bystanders — you’re part of the treatment team.
Final Thought
The TASA Study shows what many clinicians already know deep down: there’s no single solution for suicidal teens. The path forward is personal, nonlinear, and often complicated. But with patience, flexibility, and connection, recovery is absolutely possible.
When we show up consistently — not just in the crisis, but in the calm that follows — we don’t just treat symptoms. We restore hope.
🔗 Link to the study: https://pmc.ncbi.nlm.nih.gov/articles/PMC2891930/#:~:text=Based






