How to work with depression after a heart attack?
After a heart attack, untreated depression nearly doubles death risk — treatment helps patients survive.

Dr. Amir Elsamadisi
Psychiatrist & Researcher

Depression After a Heart Attack: Why Treatment Can Be Life-Saving
Description: A pivotal study from the TRIUMPH Registry (Translational Research Investigating Underlying Disparities in Acute Myocardial Infarction Patients’ Health Status), published in a major cardiology journal, followed over 4,000 heart attack survivors to examine how depression and its treatment impacted 1-year survival. The results? Untreated depression nearly doubled the risk of death, while treated depression carried no added risk. The message: Treating emotional health after a heart attack may be just as important as managing blood pressure and cholesterol.
The Takeaway
Depression is common after a heart attack — but when left untreated, it becomes life-threatening.
Among 4,062 patients with acute myocardial infarction (AMI):
- No depression: 6.1% died within a year
- Treated depression: 6.7% died (no significant difference from the no-depression group)
- Untreated depression: 10.8% died — nearly double the mortality risk
Adjusted Hazard Ratio (HR):
- Treated vs. no depression: 1.12 (not statistically significant)
- Untreated vs. no depression: 1.91 — a 91% higher risk of death
Key message: It’s not depression itself that raises risk — it’s failing to treat it.
Why Should You Care
Because depression after a heart attack can kill — but treatment can save lives.
One stat to remember: Untreated depression raised mortality risk by 91% compared to patients without depression.
The Article
This study was conducted using data from the TRIUMPH Registry, a large, multi-center observational cohort across 24 U.S. hospitals. While not a randomized trial, its size, design, and use of validated screening (PHQ-9) make it a highly credible and clinically important piece of evidence — especially for cardiologists, primary care providers, and psychiatrists.
The Clinical Data
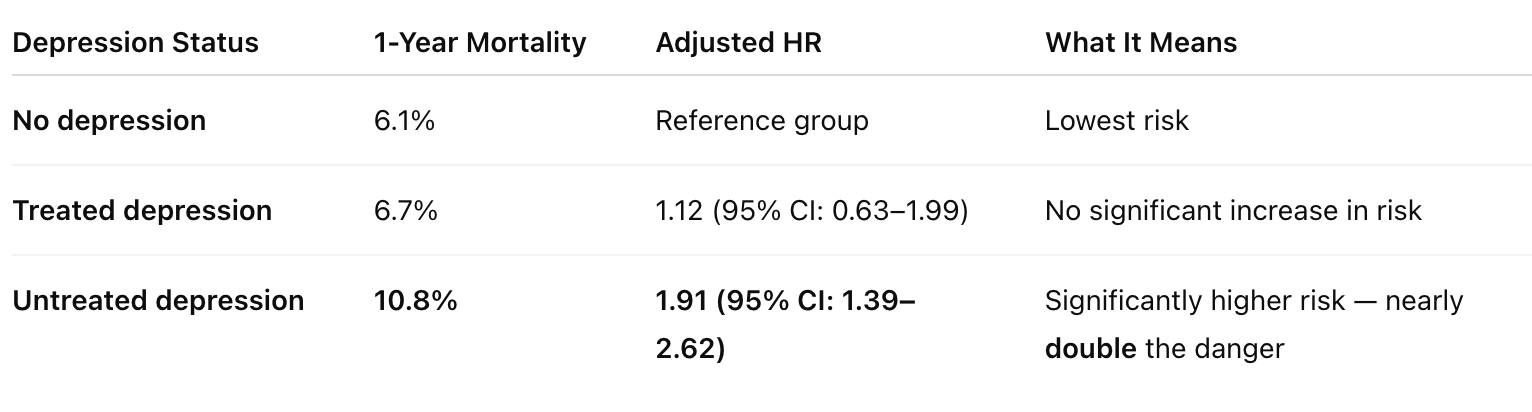
Key point: Screening alone isn’t enough. If depression is found, it must be actively treated.
Study Design: How They Figured It Out
- Study Name: TRIUMPH Registry
- Type: Multi-center observational cohort study
- Patients: 4,062 adults hospitalized for acute myocardial infarction (AMI)
- Depression Screening: PHQ-9 during hospitalization
- Treatment defined as:
- Documented diagnosis of depression
- Antidepressant medication
- Referral to a mental health provider
- Follow-up period: 1-year all-cause mortality
This was a real-world snapshot of how depression was (or wasn’t) treated in cardiac patients — and what happened next.
Why This Study Changed My Practice
As a psychiatrist, I used to view post-heart-attack depression as secondary — something we’d manage later, after stents and statins. But this study changed that.
Now I tell teams and families:
“If we screen for depression, we must treat it. Otherwise, it’s like diagnosing hypertension and walking away.”
Here’s what I do differently:
- Prioritize early depression treatment post-MI — including meds, therapy, or both
- Collaborate more closely with cardiologists
- Push for better discharge planning that includes mental health support
- Educate families that mental health isn’t just quality-of-life — it’s a survival issue
What Patients Should Know
- Depression is common after a heart attack — and it’s not a sign of weakness
- If left untreated, depression can double your risk of dying within a year
- Treatment works — antidepressants, counseling, or both can protect your health
- If you feel low, disconnected, or hopeless after a heart event — speak up
- You deserve emotional recovery, not just physical healing
Final Thought
This study reframes post-heart-attack depression not as a soft issue — but as a hard clinical outcome. Ignoring it doesn’t just prolong suffering — it increases mortality.
Mental health isn’t optional in cardiac care. It’s essential.
Let’s stop seeing depression as a side note. In heart attack recovery, it might be the turning point.
🔗 Link to the study: https://pmc.ncbi.nlm.nih.gov/articles/PMC5796757/