How Does Reimbursement Actually Work for Therapy / Psychiatry with Blue Cross Blue Shield in New Jersey?

There's a lot of information out there on reimbursement via insurance for mental health services. However, most of this information doesn't capture the real-life situations of actually using a top-tier therapist or psychiatrist.
In this article, we break down the exact process of reimbursement via a specific insurance - Blue Cross Blue Shield - for patients in New Jersey.
In this article, we have utilized as many real numbers as possible. We have noted wherever we have had placeholders.
In-Network
In Network is very simple. First, you will need to hit the deductible associated with your insurance.
Afterwards, you will pay the co-pay associated with your provider.
You will not be billed anything other than the co-pay. Once you hit your out-of-pocket maximum, you will no longer be responsible for your co-pay.
Typically, your provider will bill your insurance directly, and you will not be responsible for anything.
INSERT PICTURE HERE.
Out-Of-Network
Out of network is more complicated, as well as more common. More and more therapists and psychiatrists are no longer accepting insurance. Why? Because the rate that insurance reimburses these providers is so much lower than they typically charge.
Below, we'll walk through how billing works for an Out of Network provider.
First, you will be responsible for paying the provider directly.
Then, the provider will provide you with a "Superbill". This is the bill that you'll submit to your insurance for reimbursement.
To know how much you'll get back from your insurance, you'll need to know the following: deductible, co-insurance, out of pocket maximum, and most importantly - Allowed Amount.
How Out of Network Actually Works
Until you hit your deductible, you will be responsible for 100% of the session. Once you hit your deductible,
Once you hit your deductible, coinsurance kicks in. Coinsurance is typically a percentage - for example, 25%. Once you hit your deductible, you will be responsible for the Allowed Amount of the session * (1- 25%).
What is Allowed Amount?
Allowed Amount is a dollar rate that the insurance company determines is the amount they will reimburse for this type of procedure. Typically, for therapy sessions the Allowed Amount is ~$100. For Blue Cross Blue Shield, the Allowed Amount in New Jersey is [$90]. Many therapy and psychiatry sessions are $200 - $350 per session.
The insurance company will never reimburse more than the Allowed Amount per session - even if you hit your deductible AND your out of pocket maximum! This is something many patients do not understand when they sign up for care.
Allowed Amount is very tricky because it's difficult to find out the Allowed Amount BEFORE you sign up for your insurance plan. Oftentimes you need to call the Insurance Company to find out.
After You Hit Your Deductible and Out of Pocket Maximum
After you hit your deductible and your out of pocket maximum, your insurance company will pay 100% of the Allowed Amount for each service.
More Articles
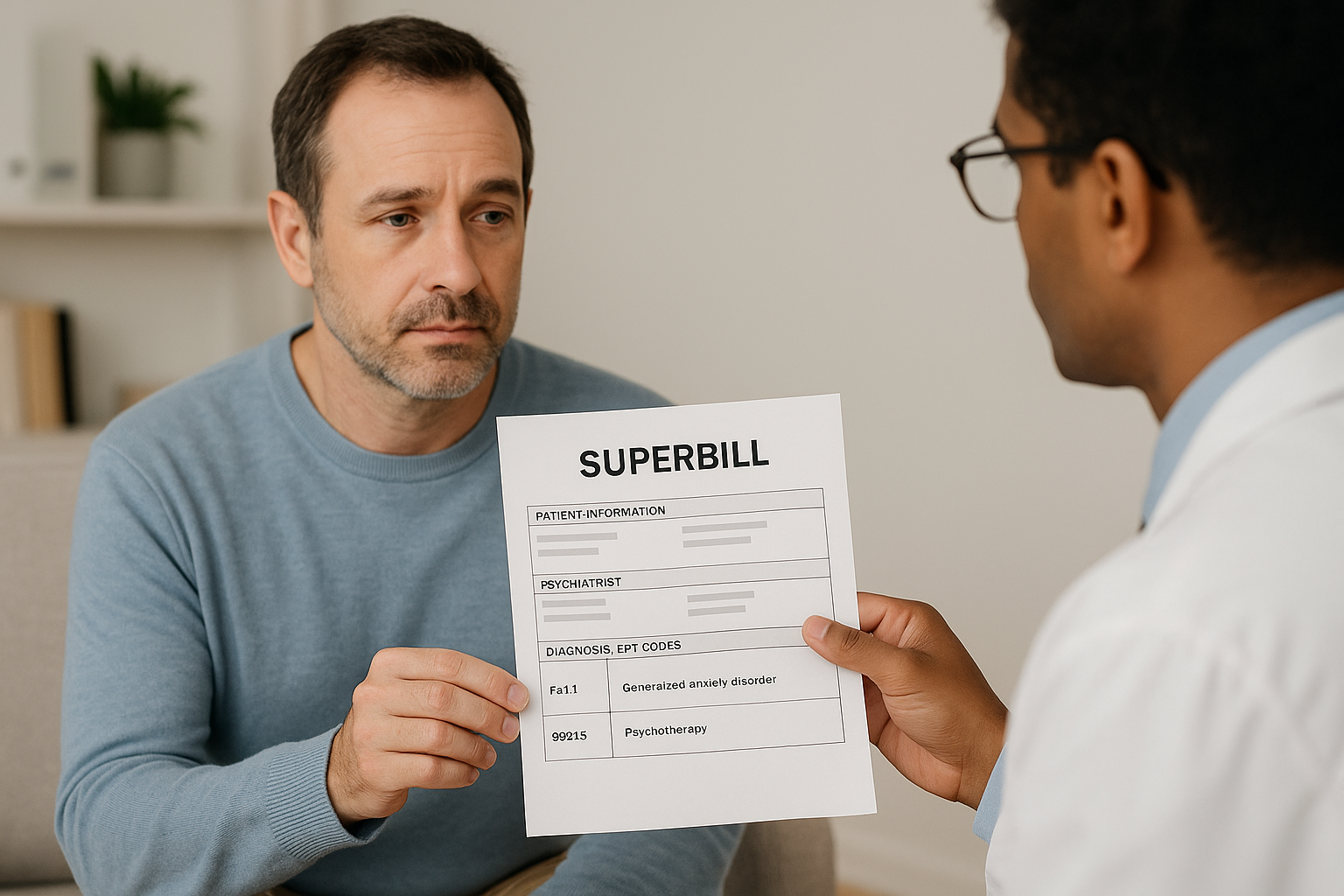
My Psychiatrist gave me a Superbill. What is that?
A simple guide to understanding superbills and getting reimbursed for out-of-network psychiatry.


